We've covered depersonalization and derealization, two of the five core dissociative symptoms. As someone with dissociative identity disorder, both of those forms of dissociation affect me regularly. But the remaining three impact my life most profoundly. Dissociative amnesia, as I'll explain, is a deeply frustrating and disruptive part of living with DID.
Living with DID
I remember a certain meeting with a girlfriend in a coffee shop. I arrived before her and sat working on a crossword puzzle while I waited. It wasn't long before she was standing next to me saying, "Hi!" I looked at her, and even though I knew my purpose in the coffee shop that day - to meet her - it took me a moment to understand who she was. It was a jarring moment in her Dissociative Identity Disorder education. "You didn't recognize me," she said. She was right. I didn't immediately recognize her, even though by then we'd spent hundreds of hours together. But it wasn't amnesia, the form of dissociation one might suspect, that prevented me from recognizing her. It was a different dissociative symptom: derealization.
What's it like to live with depersonalization in dissociative identity disorder ? Articulating the answer is challenging for me. Partly because I don't know what it's like to live without DID; partly because describing it requires a base-line level of awareness that dissociation by nature impedes. And partly because the question is so large, sort of like asking what it's like to be female. Breaking dissociation down into the five primary ways it manifests makes illuminating the experience of living with dissociative identity disorder easier. Depersonalization - the feeling that you're separate from your body - is the first.
Among those with Dissociative Identity Disorder, there's some debate about whether it should be called a disorder at all. Some even view DID as evidence of mental health. When you consider that its development is regarded as an example of adaptive functioning by many of both those who live with it and those who treat it, it's easy to understand why some might dispute the mental illness label. Mental illness by definition implies maladaptive functioning - it interferes with and disrupts daily living. But Dissociative Identity Disorder is often described as life-saving. Which is it?
Yesterday was a big day for me and my son. He started middle school. I received a painful reminder that I'd be a better mother if I didn't have Dissociative Identity Disorder and the unique memory problems that go with it.
The decision to disclose your dissociative identity disorder (DID) is a deeply personal one. Many, perhaps most, people with DID live in near silence about their disorder. They may tell only their family or no one at all. Some choose to share their dissociative identity disorder diagnosis not just with family but also friends. I belong to a smaller group of people who publicly say, "I have DID." What's comfortable for you may be unhealthy for someone else, and vice versa. With that in mind, what I offer you today isn't advice on whether or not to reveal your DID diagnosis, but a short list of DOs and DON'Ts - things to keep in mind when considering disclosure.
Living with Dissociative Identity Disorder is, among other things, lonely. I often feel like I'm watching my life as it's lived by braver or more competent others. A situation presents itself and, without conscious choice, the deck that is my system of alters begins to shuffle. Some force outside my control determines, almost instantaneously, the card best suited for the circumstances; and the card plays until the shuffling begins again. On one hand, this identity alteration is precisely what has allowed me to find employment, make friends, and parent a child. On the other, it's what separates me from the world and makes intimacy an illusion that only rarely becomes my reality.
Today, I'm pausing my discussion of the contributing factors in the development of Dissociative Identity Disorder to talk about Dissociative Identity Disorder and relationships. Navigating relationships may be the single biggest challenge I encounter living with DID. I see the havoc my disorder wreaks on my most intimate relationships and I feel helpless to do anything about it. I watch my partner in particular struggle with abandonment, loneliness, and the chaotic nature of DID and I know that more personalities doesn't always mean more love.
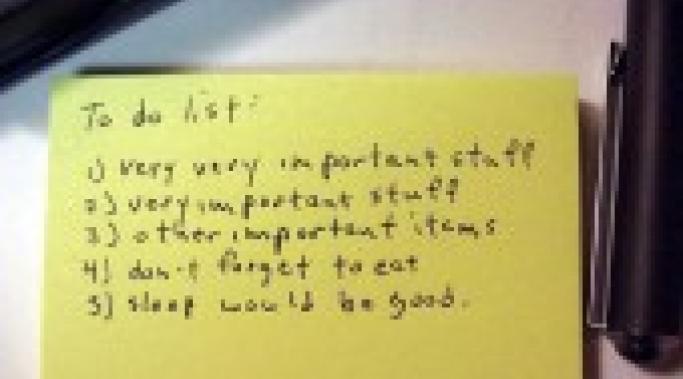
One challenge of dissociative living is task management. Dissociation creates fissures in consciousness that make the demands of daily life extremely difficult to meet. It's important that I get my son to swimming lessons on time. Showing up for psychiatric appointments is imperative. Paying bills is not optional. But I cannot expect my dissociative mind to sustain awareness of all my obligations throughout many alter states. Instead, I rely on external tools to remember for me.
My name is Holly Gray. I live in the Pacific Northwest United States with my 11-year-old son and a cat named Alex P. Keaton. My life has been a search for identity and a series of 180 degree turns that baffled and frightened me. I have been in and out of therapy since I was 14 and up until five years ago, found very few answers in the therapeutic process. I was diagnosed with Dissociative Identity Disorder in early 2005. I wrestled with the diagnosis for several years before finally coming to terms with it. In doing so, I learned and unlearned a great deal about dissociation and DID.